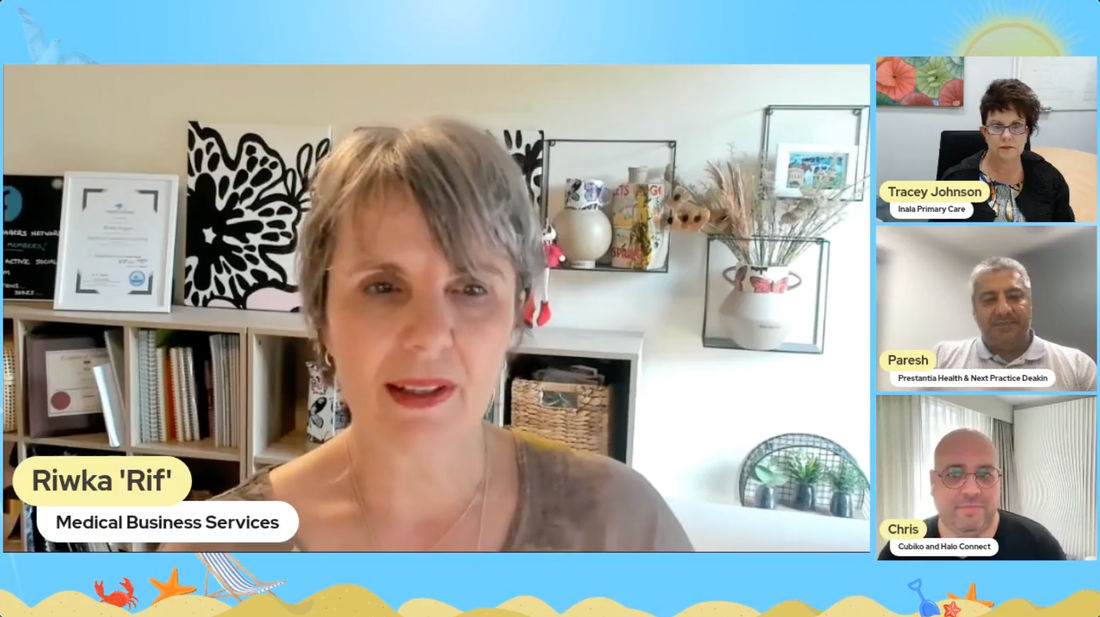
Talking HealthTech: 345 – What is the circuit breaker in general practice? Riwka Hagen, Tracy Johnson, Dr Paresh Dawda, Chris Smeed

Source: talkinghealthtech.com

Provided by:
Talking HealthTech
Published on:
28 April 2023
This is the final session of the Talking HealthTech Summer Summit, and it is one that impacts all of us, whether you are a general practitioner, or you’re creating solutions for GPs, or helping them in their business or even if you are just a human, chances are, at some point, you’ve encountered family medicine or outpatient care, and you will rely on the GP system at some point in the future.
So, this is an important one and special thanks to Best Practice Software, who are bringing you this session today. They’re one of the gold sponsors for the Talking HealthTech Summit, and they’re great supporters of THT generally.
The general practice landscape in Australia is under a lot of pressure and attention at the moment- something’s gotta give. So, what will act as the circuit breaker here to put primary care back on the right path?
This is session nine of the Talking HealthTech Summer Summit about general practice. On the panel are Riwka Hagen- a business coach, advisor and consultant at Medical Business Services, Tracy Johnson, CEO at Inala Primary Care and Dr Paresh Dawda, director and principal at Prestantia Health. Moderating the conversation is Chris Smeed, CEO and co-founder at Cubiko and Halo Connect.
General Practice Poll Question
Question: What’s the one thing that will fix general practice in Australia?
Responses: 41% of people believe GPs getting paid more will fix it all.
38% of respondents said GPs need more technology to fix it.
20% of people said if patients didn’t pay for their care, the whole thing would be fixed.
2% of people believe it’s not broken, so it doesn’t need fixing.
Meet the Panel
Riwka Hagen (Rif) is a practice management consultant. She specialises in medical business services by providing coaching, support, training and consultancy services to practices all around Australia. That also includes support for PHNs and big and small organisations all around primary care.
Dr Paresh Dawda is a GP based in Canberra and has a passion for human-centred care. He spends about half his week doing clinical work, caring for patients with complex and chronic conditions. As such, Paresh does a lot of work in the aged care, disability care and palliative care sectors. Outside of the clinical space, Paresh is also affiliated with two universities and does a bit of primary care consultancy with primary health networks, working with state and territory governments. Additionally, he has done a lot of work with New South Wales E-Health and the New South Wales Agency for Clinical Innovation and models of care.
Tracy Johnson is the CEO of Inala Primary Care which is based in Queensland. It’s a charitable GP practice with nearly forty- three people on its team. Beyond that, Tracy is a health services researcher who spends a lot of time connecting with people and running seminars as well for practices that are interested in doing care differently. She spends a lot of time telling people why general practice needs to be the core of everyone’s agenda.
Provide the Details to Alay Uncertainty
General practice is currently facing the decline and stagnation of Medicare rebates, and GPs are now agitating, including in the public media, which has rarely happened before to this extent. It’s become so evident that even the general population is surmising that something is wrong because they can’t get to see their GPs and also have to pay for the care that they’ve never had to pay for before.
So, rather than rehashing exactly what that story has led up to, the question is, what are going to be the circuit breakers for primary care?
There are going to be announcements coming up, and there have been conversations about the ten-year plan in the Medicare task force, including where funding is going to be spent. There have also been talks surrounding the government’s commitment of 750 million over the next three years, where it will be spent and the lack of clarity regarding what that commitment really means.
While GPs requested that some of the 250 million be given to them since they aren’t being paid, there has been pushback from the task force and panels, stating that the process is more complicated than that.
Right now, in order to move forward, general practice needs the detail of what’s being planned. There has been a release of snippets of information that in themselves are kind of nothing, leaving practitioners to wonder over the meaning of all these bits and pieces of information. Therefore, one circuit breaker would be to provide general practice with the details so that practices can start planning for what needs to be implemented.
Has the Change Happened?
Maybe the change has already happened- somewhat. General practice can be equated to the foot soldier of the healthcare system because these practitioners do the majority of the care in primary care and throughout the healthcare system. Yet general practice takes only a tiny little proportion, less than ten per cent of the total healthcare budget in this country.
Think about how little attention we pay to our feet, although they play such an important role. But, if we were to have blisters all about our feet from using them so much, it would become a major problem. Similarly, general practice in the public mind, and because of that, the political mind has finally become a big problem.
Additionally, the whole notion of what general practice is, is in for a fundamental change. When someone hears the term GP, they automatically assume that means a doctor. However, the revolution that is already evident and heard from the Minister for Health in the strengthening of the Medicare task force in the tenure health reform documents is that it’s actually about general practice.
From a practitioner and economist’s standpoint, it makes sense to have everyone working to the top of the scope of their licence, and this includes GPs, nurses and other allied health providers. Furthermore, because there are not enough GPs to provide care the way that it has always been done, the industry is actually being forced to look at a new model.
The new model must be team-based care and involve knowing who your patients are and doing all of the right things by that patient over the long term so that healthcare costs are not constantly being built. Instead, general practice should be providing preventative comprehensive care, which is what patients are now starting to expect and ask for.
In essence, it’s general practice’s time because the funding models and the changes that we are starting to see all point to the fact that general practice is actually now on the agenda.
Three Principles that can Circuit Break General Practice
The general practice ship has been sailing for a long time, and it’s had holes for a long time too. Eventually, water started to fill the ship, and it’s now sinking- really fast. Throughout the last twenty years, people have tinkered with primary healthcare. They’ve tried to do bits and pieces with it, most of which being pilots that come and go, but nothing really changes.
Interestingly, there are three principles that can be used in the approach to fixing the problems in general practice.
-
Today’s problems come from yesterday’s solutions. By the same token, today’s solutions might be tomorrow’s problems.
We must be careful with the reform agenda to ensure we don’t create problems for the future.
-
The easy way out leads back in.
If we’ve got a hammer, everything looks like a nail. Different members of the general practice sector believe very much in using more of the hammer (increase Medicare item numbers, increase the bulk billing, et cetera.) Maybe we need to think about different tools other than the hammer.
-
Faster is slower.
There is a sense of urgency, and something must be done quickly. But caution must be used so that in the effort to solve a problem, things don’t inadvertently get slowed down.
Therefore, in terms of a circuit breaker, we need to give a life jacket to practice sustainability, which can be done by injecting some practice-level funding as a short-term buffer while more sustainable solutions are being sought. The aim must be to create a roadmap of actionable steps that can be taken to realise the recommendations that have been made in the strengthening Medicare task force.
Other Circuit-Breaking Factors to Consider
are a few other factors that one must also consider, as they could help to shift the landscape of general practice. For one, there needs to be an in-depth discussion and decision process around bulk billing rates. There needs to be some consensus regarding who should get it or if it should even be an option.
The next factor to look at is the technology in its place because it’s such a strong enabler; however, the sector’s aspiration around the use of technology is quite limited. For example, in the strengthening Medicare task force report, there is a whole section around modernising primary care. But what it really talks about is the use of information flows, which is stuff that could have been done twenty years ago. Instead, why not use something like AI that can create intelligent insights into our data and target our clinical systems?
Technology grows exponentially, and that means technology in five years’ time will be very different to today’s technology. Unfortunately, we have a very linear perspective around the application of technology and healthcare, yet technology will continue to go up exponentially.
Bottom line- there needs to be more focus on how to create agility in innovation in primary care through having flexible funding systems, the ability for practices to be really innovative in adapting technology and not being restricted by regulatory and financial barriers, et cetera.
How Essential is Practice-level Funding?
There has been an incremental shift over time about what doctors want to take as a percentage of that revenue because, in twelve years, the Medicare extended rebate has increased by only a few dollars. Consequently, it is quite reasonable for doctors to request better payment. The fact is, inflation has halved their income over that twelve-year period.
Doctors as general practitioners are paid more than in other disciplines, and they have way less responsibility and stress. Once we get beyond the fact that GPs need to be paid more, it’s time to address the fundamentals of GPs needing a practice to operate from. If doctors are taking a bigger split of revenue, the amount of money left for practices to cover the cost of an ever-increasing rent and to award wages is far less than adequate. This takes us back to the question, “Should healthcare be free at point of access?”
The reality is that the proposed funding would still be completely insufficient to give doctors and practices more money and fund the change that must occur so that there are general practices, not homes for GPs to operate. For that transition, technology should be brought into the mix. It is also important to know who the patients are and to serve them in multiple ways. Additionally, with the shortage of GPs, there must be an increased reliance on AI, interoperable systems and on patient-fed data to allow GPs to manage them comprehensively and extensively.
Significant changes are needed within general practice, and the only way to accomplish these changes is by practices getting bundles of money that they can invest in a programmed, intelligent and nimble way. We need to stop thinking about general practice just as a Medicare-funded system and rethink practice management and operation.
This month, there is to be the announcement of practice grant funding through PHNs of up to fifty thousand dollars per practice to support IT infrastructure within practices. This is a good initiative, but at the time of this session, the details of the requirements were not forthcoming.
 Investing in Interoperability as a Circuit Breaker
Investing in Interoperability as a Circuit Breaker
In terms of interoperability and the exchange of information, healthcare is so far behind; even though we’ve been tinkering with the My Health Record system now for a number of years, it’s still a very limited functionality tool that is just not anywhere in the modern age and practitioners are nonplussed about using it because they just can’t see the benefit. Because it requires the uploading of whatever is in the system right now, it’s always old data. There is no live interaction and collation of information from various sources that provide succinct information at the point of service.
A big part of this shift and change must come back to the investment in interoperability, which also includes interoperability between the various platforms that practices use to manage their clinical and practice data. In addition, there must be an incentive to get standardisation happening there as well.
Per year, it costs about ten thousand dollars for the time that each practitioner uses to open all the systems that they need to use daily. This again goes to show that the need for interoperability is absolutely huge. Practitioners should be able to access all the systems they need to by using one login, one interoperable system through a national authentication spine. Furthermore, a lack of interoperability is actually negligent because it’s creating more of a safety risk for patients than benefits.
Monopolising Clinic Access
We must remember that healthcare is inherently political because it’s about people’s income, profile and power. So, to protect their business model, some companies are restricting access to clinics and shutting the gates on innovation and therefore preventing interoperability. But there are a couple of things that will break through this barrier.
For example, in America, they produced some legislation a couple of years ago making it illegal to have any form of software and healthcare that didn’t connect with everything else by 2025. It’s now 2023, and America has already transitioned. Also, a piece of legislation that outlines to the market that they can set their own standards, but their solutions must be interoperable could be a really powerful game changer.
A bigger share of that ‘soft infrastructure’ money could go to practices to help with care transitions because the fact is, when you look at OECD comparisons, Australia has some of the worst transitions in care. However, this is also something that interoperability could improve.
The other thing that will change the game is the move to quality, and that means reinforcing and paying practices to deliver better quality. But this should be done on the basis of population management, using smart IT, smart health service delivery models and smart tech that patients can have in their own hands as opposed to an entirely reactive healthcare system because reaction is expensive.
Circuit Breakers That Should Come into Play
In the next couple of months to a year, it would be good to see certain things happening in general practice to promote positive change. These include:
-
The release of details on funding models to allow earnest planning to take place.
-
The passing of a law allowing no new hospitals and cancelling all new hospital contracts that are in place will force the system to think about how it reinvents and does things differently, and that difference will be in primary care and general practice.
On top of that, the only thing we can control is the fact that healthcare has a cost. Who pays for it is the debate, but the only way to keep pressure on the government and to make patients understand that the cost of care is real is for practitioners to keep reflecting the cost of care in the way they bill both to Medicare and to patients. Also, there is a need to clean up the data in order to facilitate quality team-based care.

